Introduction
Entrainment is the holy grail of invasive electrophysiology. However dark its reputation among trainees – it’s a collection of fairly straightforward principles bundled together to identify and treat arrhythmia. The key to understanding and applying entrainment is keeping it very simple.
In the simplest form, entrainment is methodical manipulation of a re-entrant tachycardia circuit – i.e. disturb the tachycardia in order to understand it.Therefore the first thing that we need to understand is what is a re-entrant tachycardia and the components of it that we can manipulate.
Re-entry is one mechanism of arrhythmia and is the most fun type of mechanism. Other types include – triggered activity and automaticity (boring!)
Before digging in to entrainment, lets recap what a re-entrant circuit is. It is explained in detail here.

Playing with a single extra-stimulus : Identifying the Post Pacing Interval
In entrainment, we try to study the tachycardia by disturbing it – to do so the most fundamental component of the circuit is the excitable gap – this gap is the part where tissues are available for us to play with.

In real life, the active wavefront is very short- that why we get a sharp inscription on the recording electrode (if the wavefront was very long – the inscription would have been wide) . In contrast the refractory period is long – that’s what allows time for the mechanical function of the muslce and prevents protects from -re-excitation too fast.
This gives to the concept of diastole. By convention, diastole refer to the relaxing part of the cardiac contraction cycle during normal rhythm – which corresponds to the latter half between two QRS complexes of an ECG. Diastole in electrophysiology refers to the same interval – but the focus of attention is the intra-cardiac recording.
Therefore when we talk of diastole in EP, we are referring to the period on the intra-cardiac signal that corresponds to the latter half between the two surface R waves
Another thing to remember is that the surface ECG may not time with intra-cadiac signal as it depends on the location where the intra-cardiac signal is being recorded. The ECG may be delayed, on time or early to the EGM.
Now consider an extra-stimulus given in to the excitable gap. The paced wavefront travels in two directions – one towards the incoming tachycardia wave (which is called the antidromic wavefront) and forwards along the excitable gap (which is called the orthodromic wavefront). The antidromic wave collides with the incoming tachycardia wavefront and the orthodromic wavefront travels as the new tachycardia wavefront

As shown in the above diagram, pacing from within the tachycardia in to the excitable gap resets the tachycardia and the tachycardia continues. The post pacing interval is same as the tachycardia cycle length.
Now consider the same circuit with two electrodes – E1 and E2. What would be the observation if we pace during the excitable gap using E1?
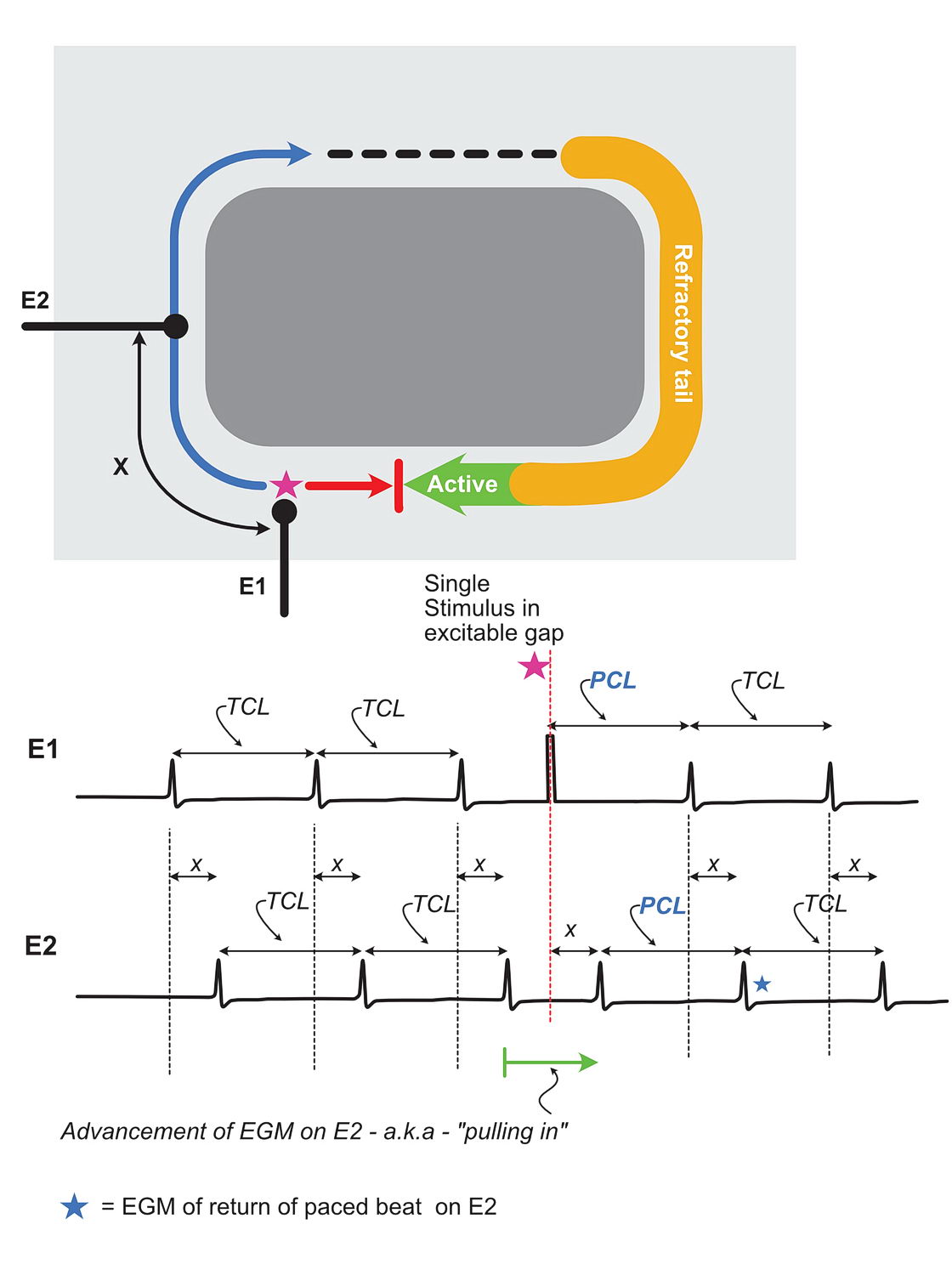
The main reason the above diagram was put here to demonstrate the importance of correctly identifying the entrained beat in other EGMs. Not only EGMs, this can by applied to surface ECGs as well. Certain pattern recognition – e.g. VAV in AVRT requires precise identification of the last entrained beat.The existence of the so called pseudo VAAV response is a direct result of failure to understand / observe the correct entrained last beat. In the above diagram the blue star represents the entrained beat on E2. Recognition of this is important to correctly calculate the PPI.
The other observation is the pulling in (aka “advancement“) of the downstream EGM. Sounds familiar ? – this is the exact thing that happens when you put PVCs during SVT to see what happens to the atrial signal. If its an AVRT and the pacing catheter is in the correct ventricle, an impulse placed during the excitable gap, will “pull” in the downstream atrial electrogram in the same way it happened in the above diagram. The post pacing interval will be same as the TCL and the tachycardia will reset and continue.
Now lets have a similar circuit – but with the electrode away from the path of the wavefront i.e. we are now out of circuit.

As explained in the diagram, when the pacing site is out of the circuit, the post pacing interval is going to be longer than the tachycardia cycle length. This is the central mechanism we use to identify a catheter position in relation to a re-entrant circuit.
Take home message :
- PPI = TCL , in circuit
- PPI > TCL out of circuit
- PPI >>> TCL waaay out of circuit !!
- PPI < TCL you are doing something wrong
Based on the post pacing interval value at various sites, we can determine the closeness of the pacing electrode to the circuit. If the PPI is equal to the TCL -bingo – we are in the circuit. If the PPI is more than the TCL, we need to look in other places and try again
Up to now this is in relation to a single extra stimulus. But the same concept can be applied to a train of impulses. The most important benefit of a train of impulses is that it gives us the ability to get into the excitable gap in any re-entrant circuit. The next section (Entrainment – 2) will discuss this in detail.
Minutiae
Understanding the core principle is more than enough to work out whats going on here. But in practice there are some things to consider.
- In real life, even dead within a circuit, PPI may not exactly match TCL – within an allowance of 30 ms is generally taken as a match
- Cardiac tissue have decremental properties. If the premature impulse is too early – it may cause decremental conduction – leading to not-perfect post pacing interval even when right in the circuit. This is seen when putting PVCs during AVRT – the AV Node decrements and increases AH interval leading to a longer post pacing interval although we expect it to be similar to to the TCL when done from the correct ventricle.
- How to find the diastolic interval to pace – by using a surrogate mark – i.e. the surface ECG or another intracardiac electrogram. Best example would be the His signal during AVRT. Pacing in time with the His signal ensures that the the tachycardia wavfront is coming towards your RV apical catheter and currently you are in the diastolic interval