Putting premature ventricular complexes (PVCs) during narrow complex tachycardia is a very useful maneuver to narrow down the differential diagnosis of SVTs.
In a normal heart, the only connection between the atrium and ventricle (vice versa) is the AV node – his bundle complex.
During tachycardia, when the His bundle is refractory (I.e. immediately after seeing a His signal on the His catheter) any disturbance placed in the ventricle should not disturb the subsequent atrial signal – unless there is an additional connection between the atria and the ventricles.
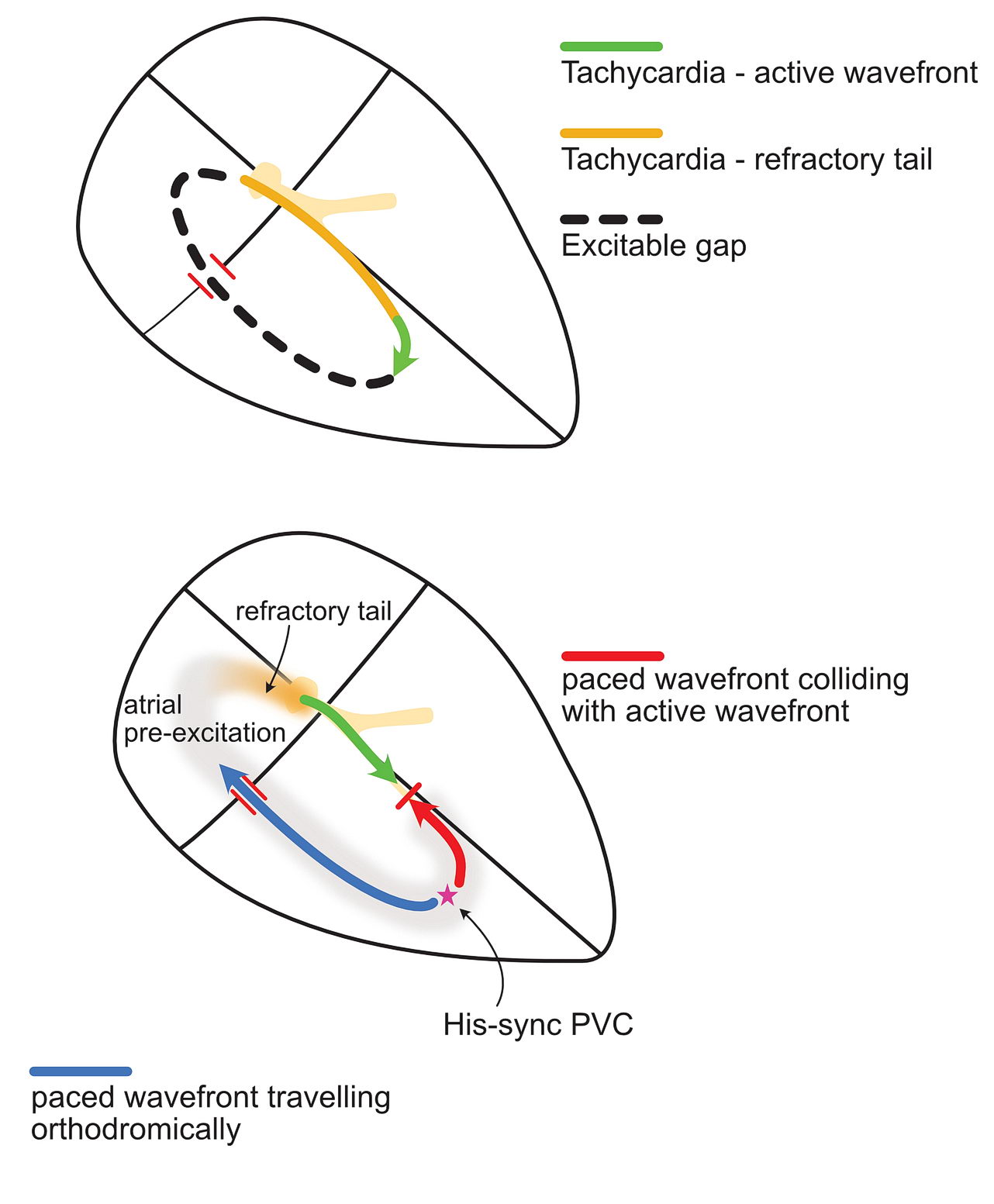
In other words, if there is an accessory pathway, putting a PVC during His refractoriness should change the timing of the next atrial signal as the PVC can ascend to the atrium via the accessory pathway. Look at the following diagram:
Why do we time it with the His signal? – because then we are sure that the His bundle is refractory i.e. unable to conduct.
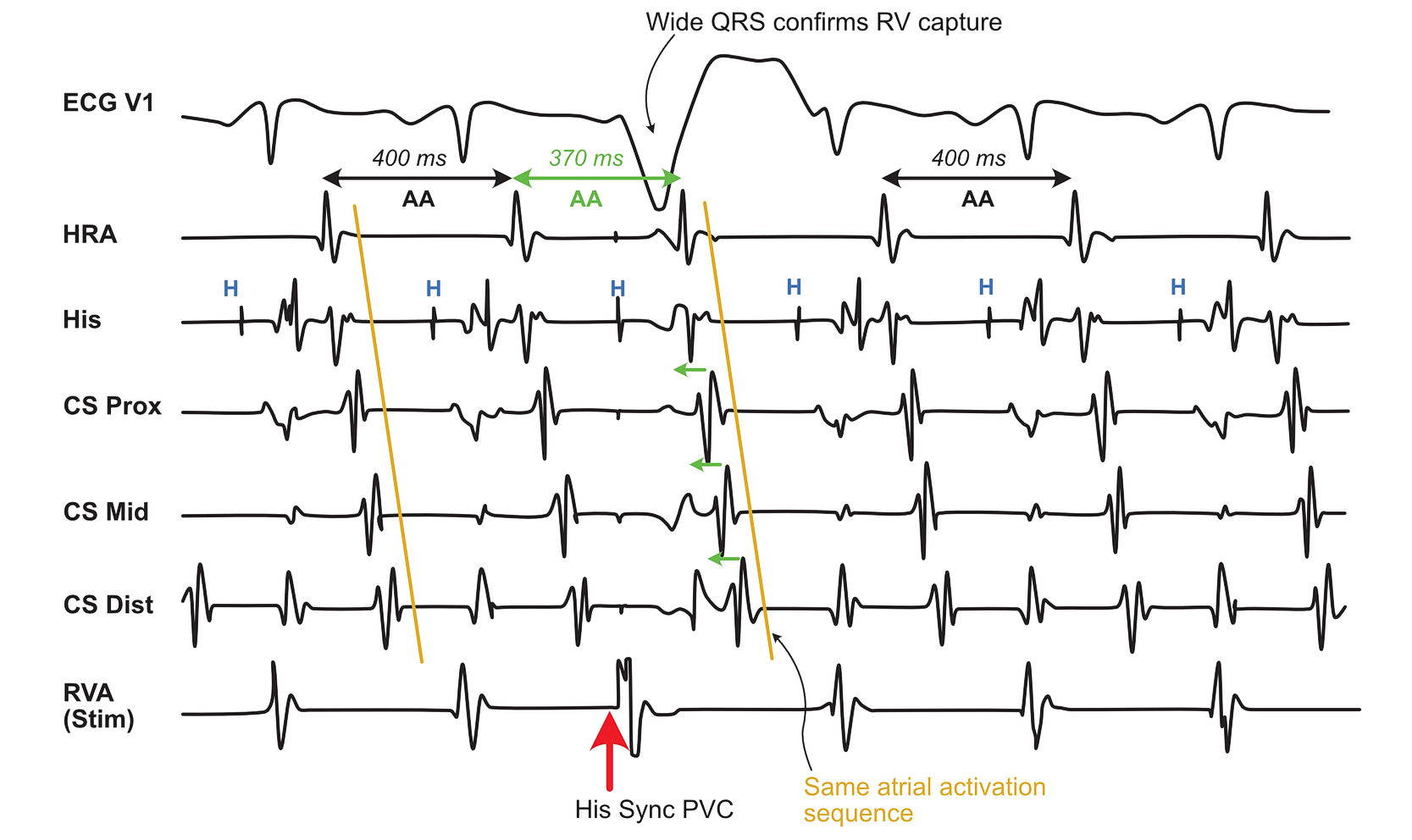
Now lets look at an example tracing and study this further. Also recommended to read this section on entrainment as this is really got to do with entrainment. If you understood that – this is not a mystery.
As shown in the diagram, the advancement of the atrial signal confirms the presence of the pathway. To really prove that this pathway is participating in the tachycardia is by proving resetting as AVRT would be a re-entrant tachycardia.
Why do we need to prove it? Because if the pathway is a bystander, and the tachycardia is something else – we would be in trouble. Admittedly bystander pathways are rare – most of them do participate in the tachycardia – but knowing the principle of resetting and looking for it helps when faced with rarity !
Lets add some more measurements to the tracing :

In real life, proving reset is difficult as the intervals are subtle. The advancement of the atrial signal with the same atrial activation sequence is good enough to say that the tachycardia is AVRT. However if the activation sequence has changed, then you may be dealing with a bystander or a pathway to pathway tachycardia
However, termination of tachycardia without an atrial signal proves that the tachycardia is indeed AVRT. Lets look at a schematic and a tracing.


Occasionally, one may observe the next A getting late – this is because the early PVC decrements in the accessory pathway. This type of APs are rare and can lead to incessant tachycardia as in persistent junctional re-entrant tachycardia – mostly seen in kids
This delayed A response is unique that it self proves the presence of the pathway AND its participation in tachycardia.
Since the pathway decrements, the VA interval (and therefore the RP interval on the ECG) is long and therefore PJRT comes in to the differential diagnosis of long RP tachycardia. This is discussed later.
Rarely, the post pacing interval may be very long – despite other evidence of accessory pathway conduction ( i.e. Pulled in A, same atrial activation sequence, Extra-nodal response in Parahisian pacing) – this could be due to the return beat coming down via a slow AV nodal pathway.
Practically how would you time the PVC?. Basically one selects a good surface ECG and times the delivery of the impulse by scanning back in decrements of 10 ms. The stimulator will calculate the position based on the sensed R wave and deliver the impulse. Generally a several tries need to be done and the EGMs carefully inspected for proper timing.
The impulse should be always delivered exactly when the His signal seen or before its inscription (within 20 ms) . This is ensures that the His is indeed depolarized and refractory.
The other thing to be sure is proper ventricular capture. This easily confirmed by a large QRS spike from the paced beat. However at times there is no RV apex catheter and ventricular pace is from the His distal – where the ventricular capture may be narrow and difficult to identify.

So what about other forms of SVTs – ATs? AVNRTs? – in either of these, there is no obligatory connection between the atria and the ventricles to sustain tachycardia – hence His synchronous PVC has no effect – Unless there is a bystander pathway – which is not participating in the tachycardia – how would we suspect it – is by looking at both – the atrial advancement and activation sequence. (The atrium would advance but the activation sequnce would be different and there won’t be any resetting of tachycardia)

His synchronous PVCs for narrow complex tachycardia
Take home messages :
- Termination of tachycardia – without A, confirms presence of AP AND its participation in tachycardia
- Advancement of A (pulled in A) – confirms presence of AP but does NOT prove its participation.
- Resetting and same activation sequence add evidence for pathway participation
- Delayed A (pushed A) – confirms presence of decremental AP AND proves its participation in tachycardia.