Spontaneous occurence of a bundle branch block during narrow complex tachycardia can give a clue to its etiology as well as help determine the side of an accessory pathway if there is evidence for such.
Lets assume that there is a narrow complex tachycardia going on and a left bundle branch block develops. If the tachycardia cycle length is more during the tachycardia, that indicates that the tachycardia is AV re-entry and there is a pathway on the left side. Lets look at the following diagram:

From the above diagram, it is a readily apparent how a bundle branch block prolongs the cycle length of an SVT – and this indicates the presence of an accessory pathway on the side of the bundle branch block (i.e. LBBB would indicate a left side AP and RBBB would indicate a Right side AP) . The main observation is the increased cycle length during tachycardia. This would not happen with a bundle branch with other SVTs (e.g. Atrial tachycardia with a left bundle branch block).
The above discussion states that we need to carefully measure the cycle length – which could be a problem on the surface ECG if retrograde Ps are not seen properly. That’s the reason why this observation is preferably made using intra-cardiac electrograms
The other reason that we need to have the electrograms is to assess the VA interval. As the above diagram showed, the principle change is the VA interval – which subsequently affects the tachy cycle length (TCL). However at times, the decrease in VA interval when the bundle branch block resolves, is compensated by an increase in the AH interval as the AV Node decrements – this leads to only small overall changes in the tachycardia cycle length. Therefore it is essential that we show a change in the VA interval to confirm our assessment
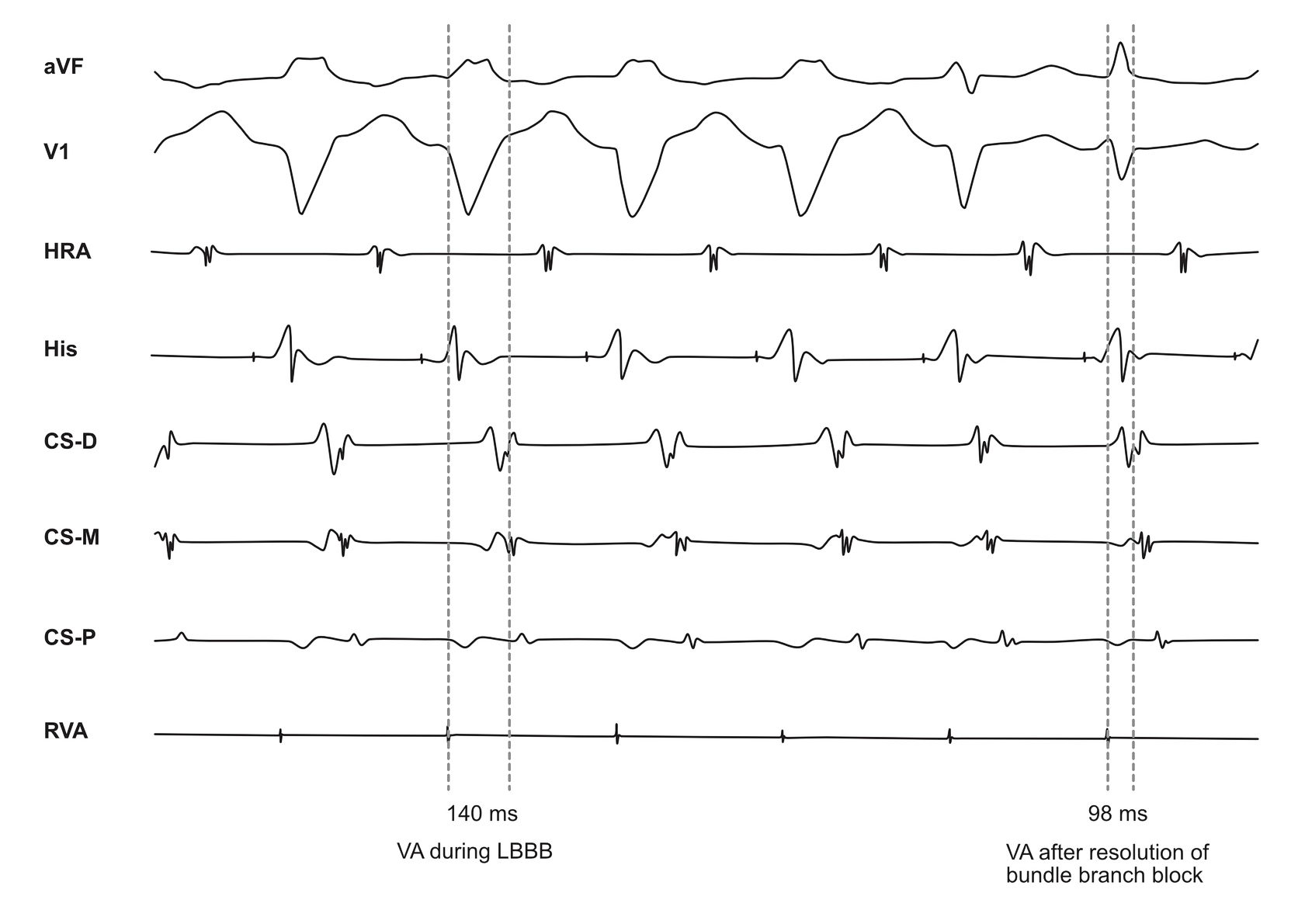
In the above example, the overall tachycardia cycle length change is very subtle. However, there is a dramatic change in the VA interval upon cessation of left bundle branch block. This highlights the need to look for the change in VA interval – not the TCL.
The absolute value of VA change may also help localization. It is said that a VA interval change less than 30 ms during LBBB is suggestive of a postero-septal AP (which may be left or right, but most of the time ablatable from right) . More than > 30 ms change is suggestive of a free wall location.
A prolongation of VA interval during narrow complex tachycardia with an accompanying bundle branch block pattern indicates that the tachycardia is an AVRT and the pathway is on the same side as the bundle branch block