Pre-excitation index is a measurement derived from a maneuver done during narrow complex tachycardia to differentiate between AV nodal re-entry and AV re-entry from an accessory pathway. Additionally the numerical value gives a clue as to the potential site of the accessory pathway.
The principle behind the index is to get the distance from the pacing site to the tachycardia circuit based on the ability of a premature impulse to get into the excitable gap.
The original description (by Miles et. al.) stated – “pre-excitation index is the difference between the tachycardia cycle length and the longest coupling interval a premature ventricular impulse could pre-excite the atrium during tachycardia” Lets dissect the statement with the following series of diagrams.
Lets assume that there is an orthodromic AVRT going on based on a right side accessory pathway
We have a catheter in the RV apex and we start putting premature impulses – first at near the next beat and progressively with shorter coupling interval. For argument’s sake lets assume that the pacing catheter is in the circuit.
We start putting premature PVCs and when very close to the tacycarida cycle length, the PVC cannot enter the circuit as it meets refractory tissue. Therefore it is clear that the PVC has to come in earlier and earlier to find the excitable gap. (Very early PVCs would terminate the tachycardia by colliding with the tail of the previous cycle.)

So when we progressively shorten the coupling interval, the PVC finds the excitable gap and pre-excites the atrium. At this point, it is apparent that it is basically resetting the tachycardia and the paced wave would go around the circuit it and come back to electrode in the native tachycardia cycle length. (This exactly similar to what we saw in Entrainment – 1)
In other words, the PVC with the longest coupling interval which captures excitable gap and pre-excites the atrium represents a PVC which has managed to get into the excitable gap at its tail end (i.e. just before the next active wavefront). From the diagram it is apparent that at that point the TCL by the paced PVC has to be equal to the TCL – i.e. the post pacing interval has to be equal to the tachycardia cycle length.
But whats special about entering the excitable gap at its very end ? – because that will prevent an excessively short coupling interval to the AP – in other words we prevent decremental conduction in the AP by keeping the paced cycle length as close as possible to the native cycle length. As described below, the most value of this maneuver is to identify septal pathways – of some which can be decremental. Therefore a random PVC might be too early to the AP causing decremental conduction.

The pre-excitation index statement requires us to substract the longest PVC coupling interval (V1V2) from the TCL (V1V1). In theory, if we are in the circuit AND in the excitable gap, the numerical value would be zero (similar to PPI-TCL).
But in practice we are at the RV apex and therefore out of circuit. Since we are exactly aiming to the end of the excitable gap, any difference in the V1V1-V1V2 should represent the distance which the PVC has to travel to enter the circuit.
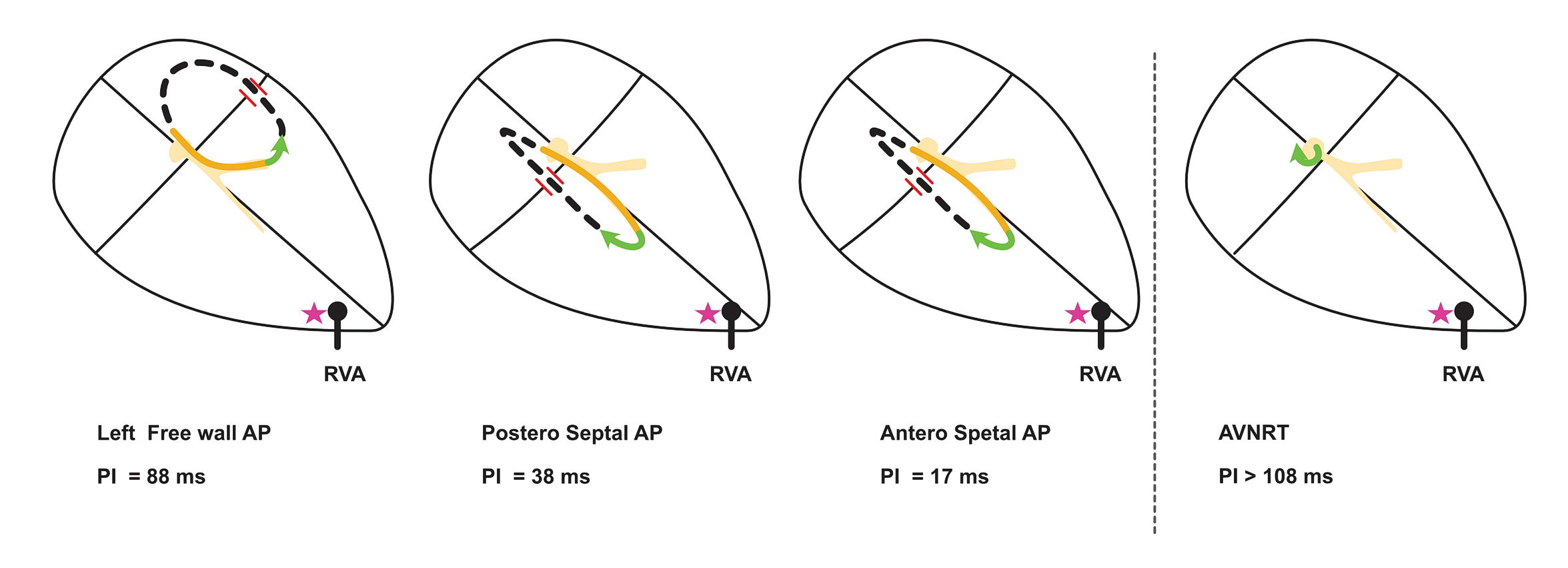
As per the original description, Miles et.al. found out that a antero-septal APs had the least pre-excitation index (a mean of 17 ms) explaining their closeness to the pacing site. Postero septal APs were a bit away and therefore their mean pre-excitation index was 38 ms. In comparison, left free wall APs had a large pre-excitation index of 88ms. They also saw apparent pre-excitation of AVNRTs ( which is theoretically possible if the pace manages to get into the excitable gap in the AVNRT circuit). However this was associated with pre-excitation index of > 108 ms, not surprising given the distance needed to travel to get into the circuit.
Therefore pre-excitation index is a useful maneuver to confirm and get a clue as to the location of a given AP. (Mainly differentiate between posteroseptal and other APs)
The reason why we look for the longest coupling interval that pre-excites the atrium is to find the end of the excitable gap for the PVC to enter without decrementing the AP