Purpose
To identify the presence of an extra-nodal connection between the atria and the ventricle – i.e. an accessory pathway (complementary to parahisian pacing maneuver)
Why ?
- Useful maneuver in sinus rhythm when the presence of a concealed accessory pathway is suspected
- Post ablation, to confirm complete abolition of retrograde conduction in an accessory pathway.
- As a complementary procedure to confirm findings of parahisian pacing
Technique
In normal a heart without any extra-nodal AV connection (i.e. no AV accessory pathways), the exclusive connection between the atria and the ventricles is via the His bundle
In a normal person without any accessory AV connection, if one paces at the base of the ventricle (i.e. near the tricuspid valve) the impulse takes a certain time as it has to travel intra-myocardially to reach the right bundle terminus and then penetrate retrograde via the His bundle
In the same person if the pacing is done near the RV apex – where it is closer to the right bundle terminus, the time to reach the atrium would be less compared to pacing at the base.
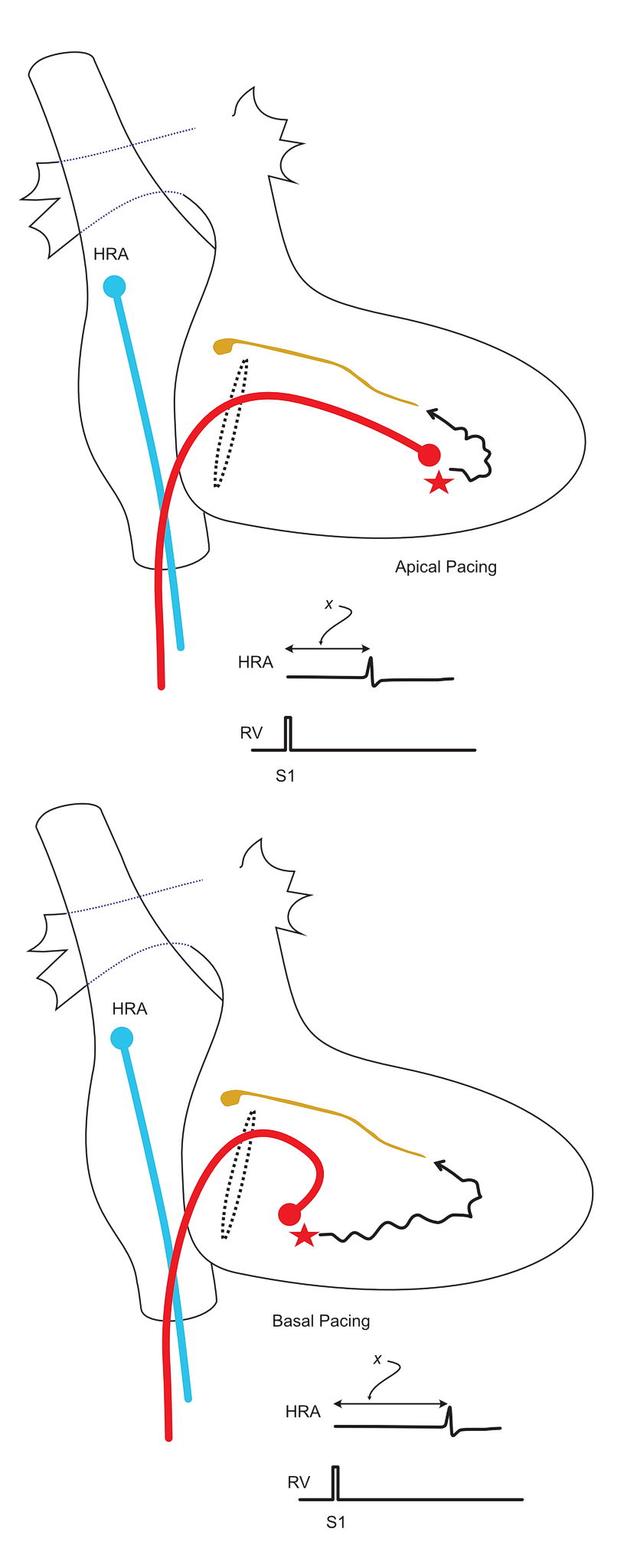
However, in a patient with an accessory pathway, since the pathway “leaks” current in to the atrium, the stimulus to atrial time in the base is going to be lesser than in when paced in the apex

Essential Aspect : Proper placement of pacing catheter in the base of the RV. This is best done in RAO 30 view.
Differential pacing thus helps to identify a retroradely conducting pathway – similar to parahisian pacing. Parahisian pacing depends on having a similar stimulus to A time when direct his bundle capture is lost – however this distinction is based on the observation of a difference in QRS morphology – which at times can be very challenging to see. In such situation, differential pacing is valuable to confirm the parahisian pacing findings.
Similar to parahisian pacing, this maneuver also can be falsely negative for left sided pathways unless the pacing catheter is on the left side.
Compared to parahisian pacing, however direct atrial capture is unusual unless the catheter placement is very annular.
In practice, this maneuver is most useful after ablation – as the ablation catheter is steerable to the base and apex for pacing. Even in overt WPW patients, after an apparently successful ablation (i.e. loss of pre-excitation – delta wave), the retrograde component can remain – which can lead to tachycardia. This is where this maneuver is very useful – again in complementary with parahisian pacing